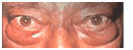
Ptosis – upper eyelid drooping
Ptosis is the term used for drooping of the upper eyelids. There are two types: congenital ptosis, which is more common, and acquired ptosis. Ptosis may involve one or both eyes and ranges from mild to severe. In cases of mild ptosis, the eye has an undesirable appearance but is functionally normal. In severe ptosis the drooping upper lid covers the pupil and visual axis of the eye, so the patient must lift his or her chin to see properly.
Congenital Ptosis
Congenital ptosis is present at birth and results from the poor development of the levator palpebrae superioris muscle, which lifts the eyelid. A child may have ptosis alone or may have other associated eye abnormalities such as eye movement disorders, refractive disorders and neurological disorders.
Acquired Ptosis
Acquired ptosis may occur at any time after birth, but is more common in old age. The etiology of this form of ptosis is normally ascribed to the weakening of the levator palpebrae superioris muscle due to such factors as old age, injury, surgery, muscular disease and neurological disease.
Symptoms
- Drooping of the upper eyelid of both eyes; it may be mild or severe enough to cover the cornea.
- Tired appearance of the eyes
- Undesirable facial appearance due to drooping of the upper eyelid
- Elevated chin, in cases of severe ptosis
- Poor vision due to associated refractive errors
- Stiff neck due to constant chin elevation
- Decreased vision when the droop is severe and covers the pupil.
Treatment
Ptosis results in an undesirable facial appearance. Normal vision is affected in severe ptosis, thus hindering the daily activities of the person. Treatment is necessary even in cases of mild ptosis in order that the patient has the opportunity to lead life as a normal person. A child suffering from ptosis has a psychological handicap when compared to other normal children. Hence, severe cases should be treated as early as possible; otherwise, ptosis may lead to abnormal head positions or decreased vision. Treatment provides a desirable facial appearance as well as normal vision.
Surgery
The treatment is surgery. It usually involves one of the two procedures: strengthening the levator palpebrae superioris muscle or lifting the eyelid mechanically with the help of a thread-like material called a sling. Levator surgery is done in cases of mild or moderate ptosis, while sling surgery is performed in cases of severe ptosis. The levator muscle is strengthened by surgery so as to allow it to lift the eyelid normally.
Postoperative period
During the initial period after surgery, the patient may not be able to close his or her eyes fully, even during sleep. This malfunction results in a frightening appearance, but is usually corrected within a few weeks. Furthermore, when the patient looks down, the white of the eye may be visible. The patient is trained to move his or her head to look down rather than to move only the eyes.
Prognosis
The surgery for ptosis is quite safe and effective.
Risks of ptosis surgery
Generally, the surgery is safe. However, complications such as infection, bleeding, reduced vision, reduced eye movement, and corneal ulcer, may occur. The aim of the surgery is to have equal lid height in both the eyes. Under-correction or over-correction may occur, but either mistake can be rectified.


Eyelid skin cancer
The skin of the eyelids and the adjoining areas of the face may develop cancer. Most commonly the cancer involves the lower lid, but it may present in other regions such as the upper eyelid, corners of the eye, eyelid margins, eyebrow skin or adjacent areas on the face.
Persons likely to get skin cancer
Eyelid skin cancer is more common in the elderly. Fair-skinned people develop skin cancer more frequently. Excessive exposure to sunlight is an important contributory factor to skin cancer.
Symptoms
- Painless elevations or nodules on skin
- Growing nodules or elevations
- Nodules, elevations or moles which become painful
- Distorted or missing eyelashes
- Ulceration, along with bleeding, crusting or distortion of the skin, especially on pre-existing nodules, elevations or moles
Types of eyelid skin cancer
- Basal cell carcinoma (most common)
- Squamous cell carcinoma
- Sebaceous gland carcinoma
All types of eyelid skin cancer may spread very slowly to other parts of the body. If the tumor is detected early enough, excision of the involved skin of the eyelid can cure the patient of the disease. However, if the treatment is delayed or is incomplete, there is a chance that the cancer may spread to other parts of the body.
Treatment
Excision of the eyelid cancer involves two principles: removal of the affected area and reconstruction. Removal involves cutting out the affected skin; at times, this means that the whole eyelid has to be sacrificed. After removal of a cancerous growth, a defect remains in the lid. Repair of this defect is known as reconstruction. The aim of reconstructive surgery is to re-form an eyelid so that it functions properly – that is, it protects the eye, preserves vision and restores normal appearance to the eyelids.
Biopsy
Biopsy confirms or rejects the clinical suspicion that the growth is cancerous. If a tumor is large, a piece of it is removed and sent to the pathologist to identify the type of cancer. Using this piece of tissue, information about the type of cancer and chances of its spread is ascertained. The preferred treatment is then decided upon. If the tumor is small, it is resected fully and then sent to the pathologist.
Reconstructive surgery may require tissue grafting to compensate for the tissue loss that results after excision. This graft is taken from any of the following regions: the other eyelid of the same eye, eyelid of the other eye or facial skin.
Excision of the tumor and reconstruction of the eyelid are usually done in the same operation. In a few cases, however, further surgery may be required after to provide a cosmetically acceptable appearance to the eyelids.
Postoperative condition
A scar remains after eyelid surgery. An effort is made to make the scar as minimal as possible. Regular follow-up visits are essential to ensure that the eyelid tissue remains healthy. If the tumor recurs, it is identified and treated as soon as possible.
Thyroid eye disease
The eye is located in a bony socket known as the orbit. In addition to the eyeball, the orbit contains muscles (which move the eye), the optic nerve (which sends visual signals to the brain) and fat. In thyroid eye disease the amount of fat in the orbit increases and the muscles thicken. As a result of these changes, there is forward protrusion of the eyes. The protrusion stretches the optic nerve and, in extreme cases, may damage it. If the protrusion is too great, the lids may not cover the cornea and corneal ulceration may result. The muscles lose some of their functional ability due to abnormal thickening, possibly leading to squinting of the eye.
Thyroid eye disease occurs primarily in people suffering from thyroid disorders, which result either from excessive or diminished production of the thyroid hormone.However, some people may have this disease with a normally functioning thyroid gland. The disease usually occurs in middle age persons of 40-50 years. Women are more likely to be affected than men.
Symptoms
- Dryness of the eye
- Swelling of the upper and lower eyelids
- Frightened or staring look
- Forward protrusion of the eyeballs
- Inability to close the eye
- Decreased vision when optic nerve is affected
- Double vision and decreased eye movements when eye muscles are affected.
Investigations
The presence of thyroid eye disease is confirmed by orbital ultrasound. If this test cannot be performed, a CT scan may be required. In addition, any person suspected of having thyroid eye disease should undergo a blood test to ascertain whether the thyroid hormone level in the blood is higher or lower than normal.
Treatment
Treatment is essential to protect the cornea and the optic nerve from getting permanently damaged. In the initial stages of the disease, lubricating drops are used to keep the eye moist. Most patients must be started on steroid tablets for a few months to control the progression of the disease. Closure of the lids may be required if the lids are not able to completely cover the eyes. The closure is temporary and is done only on the outer part of the lids, leaving the cornea clear so that vision is not affected. If protrusion of the eyeball is too great the optic nerve is in danger. At this stage, orbital decompression is advised. This surgery involves breaking one or more walls of the orbit in order that the extra fat, which has been deposited in the orbit due to thyroid eye disease, may be displaced out of the orbit. The eyeball can then be pushed back into the orbit. A patient who has suffered from thyroid eye disease for a long time develops eye movement disorders and requires eye muscle surgery to regain proper functioning of the muscles and to treat squint.
Risks of treatment
Steroid tablets may cause gastric irritation, weight gain, a puffy face, and interference with blood sugar control in diabetes. Therefore, these drugs are prescribed in as low a dose as possible. Only a few patients are not able to tolerate this small dose; in such patients surgery is advised. Orbital decompression surgery is safe, but in rare cases causes bleeding, infection, decreased eye movement, and loss of vision.
